Understanding Peripheral Arterial Disease
When Leg Pain Means Something More: Understanding Peripheral Arterial Disease
by Aaron Litvak
What is Peripheral Arterial Disease (PAD)?
Many people often assume that aching legs are just a natural part of getting older. Soreness after a long day, discomfort on walks, or needing to rest more often – these all seem like minor inconveniences. But when leg pain becomes persistent during exercise or walking with relief after rest, it could be a sign of something more serious.
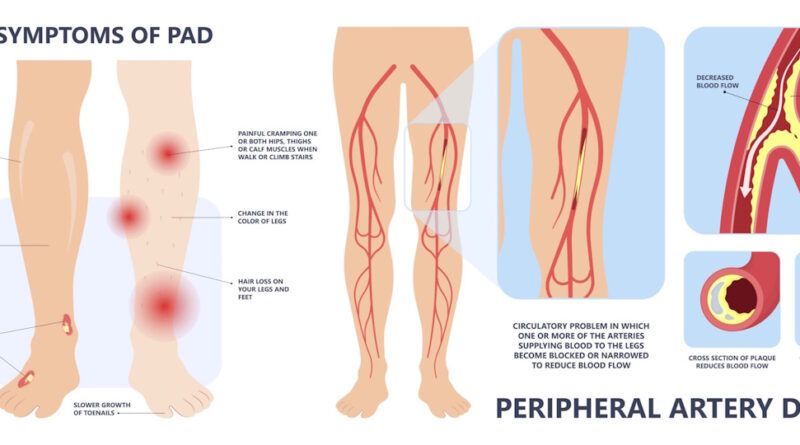
Peripheral arterial disease (PAD) is a condition that affects blood flow to the legs and feet. It occurs when plaque builds up in the arteries, narrowing them and making it harder for blood to reach the limbs (1). PAD is more common in people who smoke, have diabetes, or have high blood pressure or cholesterol. These conditions can all constrict and damages blood vessels making them more prone to build plaque and provide less blood to the muscles in the legs (2, 3).
The Warning Signs of PAD
The most common symptom of PAD is leg pain while walking that improves with rest (2). This pain, known as claudication, usually affects the calves but can also occur in the thighs or buttocks, since these major muscles move our legs and require consistent blood flow to provide oxygen and energy. Once blood flow is reduced, muscles will ache much sooner than in someone without PAD (3). Other signs include one foot that is colder than the other; slow-healing sores or wounds on the legs or feet; numbness; or skin discoloration including pale, blue, or shiny (1).
These symptoms can often be mistaken for arthritis or general muscle fatigue. However, pain that consistently appears with activity and disappears with rest is a key indicator of circulation problems. Left untreated, PAD can lead to serious complications such as infections, ulcers, and even amputation (3).
Getting Checked and Taking Action
Diagnosing PAD is straightforward. A simple test performed by medical professionals called an ankle-brachial index (ABI) compares blood pressure in the legs and arms. A significant difference between the two can indicate poor circulation into the legs (1). Additional imaging tests, such as ultrasounds, can provide further details.
Fortunately, lifestyle changes can help manage the condition. Quitting smoking; eating a healthy diet of foods low in fat, sugar and sodium; and regular exercise can all slow disease progression (4). In many cases, medications to lower cholesterol, blood pressure, or better control diabetes may be needed (2). Other patients may need medications such as aspirin or cilostazol to improve blood flow, medical procedures such as balloon angioplasty to restore circulation, or conventional surgery to open and unblock arteries (1, 4).
Recognizing PAD early can prevent serious complications (4). If leg pain interferes with daily activities, it is important to seek medical advice. What may seem like a minor inconvenience could be an early warning sign of a larger health issue. However, early recognition of symptoms and working with your healthcare providers may improve outcomes and limit progression of symptoms with a variety of treatment options (1).
References:
- https://vascular.org/your-vascular-health/vascular-conditions/common-conditions/peripheral-artery-disease
- https://www.cdc.gov/heart-disease/about/peripheral-arterial-disease.html
- https://www.ncbi.nlm.nih.gov/books/NBK430745/
- https://my.clevelandclinic.org/health/diseases/17357-peripheral-artery-disease-pad
Aaron Litvak is from Livingston, New Jersey and is currently a third-year medical student at the University of Rochester School of Medicine and Dentistry and attended college at Cornell University where he studied biological sciences and history. He is part of the school’s “LatinX Health Pathway” and is also a leader within the Vascular Surgery Interest Group. His experiences growing up speaking another language influenced him to make medicine and healthcare as accessible and understandable to the Spanish speaking community as possible. Aaron hopes to pursue a career in vascular surgery after medical school.
Medicine and Dentistry and attended college at Cornell University where he studied biological sciences and history. He is part of the school’s “LatinX Health Pathway” and is also a leader within the Vascular Surgery Interest Group. His experiences growing up speaking another language influenced him to make medicine and healthcare as accessible and understandable to the Spanish speaking community as possible. Aaron hopes to pursue a career in vascular surgery after medical school.